最近一期的Nature上的蛋白质组学文章
丁香园论坛
8249
大家都知道蛋白质组学的方法可以用来寻找药物靶点,但是对于如何寻找药物靶点,如何确证药物靶点这些具体的东西还没有
一个清晰的轮廓,这使得蛋白质组学在药物靶点寻找方面还停留在概念上。而最近Nature上的一篇文章是我们看到一线曙光。
Sidney Kimmel癌症研究中心的SCHNITZER 领导的研究小组采用削减蛋白质组作图的方法加快蛋白组学寻找药物靶点的工作。
Nature 429, 629 - 635
PHIL OH, YAN LI, JINGYI YU, EBERHARD DURR, KAROLINA M. KRASINSKA, LUCY A. CARVER, JACQUELINE E. TESTA & JAN E.
SCHNITZER
Sidney Kimmel Cancer Center, 10835 Altman Row, San Diego, California 92121, USA
Correspondence and requests for materials should be addressed to J.E.S. (jschnitzer@skcc.org).
Subtractive proteomic mapping of the endothelial surface in lung and solid tumours for tissue-specific therapy
The molecular complexity of tissues and the inaccessibility of most cells within a tissue limit the discovery
of key targets for tissue-specific delivery of therapeutic and imaging agents in vivo. Here, we describe a
hypothesis-driven, systems biology approach to identifying a small subset of proteins induced at the tissue–
blood interface that are inherently accessible to antibodies injected intravenously. We use subcellular
fractionation, subtractive proteomics and bioinformatics to identify endothelial cell surface proteins
exhibiting restricted tissue distribution and apparent tissue modulation. Expression profiling and
-scintigraphic imaging with antibodies establishes two of these proteins, aminopeptidase-P and annexin A1, as
selective in vivo targets for antibodies in lungs and solid tumours, respectively. Radio-immunotherapy to
annexin A1 destroys tumours and increases animal survival. This analytical strategy can map tissue- and
disease-specific expression of endothelial cell surface proteins to uncover novel accessible targets useful for
imaging and therapy.
New targets are needed for detecting disease through molecular imaging1-4 and for treating disease through
directed delivery in vivo5-9. Sequencing the human genome has identified a target pool of 40,000 genes which
may translate into a million possible protein targets10. Genomic and proteomic analysis of normal and diseased
tissues has yielded thousands of genes and gene products for diagnostic and tissue assignment as well as
potential therapeutic targets5-11. But the shear number of candidates can overwhelm the required in vivo
validation process, leading some to question the ultimate impact of these approaches on speeding up drug
discovery5-7, 10. Reducing tissue data complexity to a manageable subset of candidates most relevant to
targeting, imaging and treating disease is clearly desired but requires new discovery and validation
strategies, that effectively focus the power of global identification technologies.
Selectively targeting a single organ or diseased tissue (such as a solid tumour) in vivo remains a desirable
but elusive goal for molecular medicine12, 13. This targeting would allow more effective imaging as well as
drug and gene therapies for many acquired and genetic diseases1-4, 6, 7, 10-13. Most tissue- and
disease-associated proteins are expressed by cells inside tissue compartments not readily accessible to
intravenously injected biological agents such as antibodies. This inaccessibility hinders many site-directed
therapies5-7, 12, 13 and imaging agents1-4. For example, multiple barriers to delivery prevent effective
immunotherapy for solid tumours in vivo, despite efficacy and specificity in vitro12-17. Conversely, the nearly
universal access of chemotherapeutics dilutes efficacy requiring increased dosages, leading to unwanted
systemic side effects. Thus, new approaches are required to filter the overabundance of molecular information
to allow rapid discovery and validation of accessible tissue-specific targets that can direct molecular imaging
and pharmacodelivery in vivo.
Here, we divert analytical focus from the poorly accessible cells inside tissues to the critical tissue–blood
interface, inherently accessible to agents absorbed or injected into the blood. The endothelium is a minor
tissue component that exists as an attenuated cell monolayer lining all blood vessels and is in direct contact
with the circulating blood. The tissue microenvironment surrounding blood vessels seems to control the
endothelial cell phenotype in vivo18-22. But the degree to which normal and diseased tissues can modulate
endothelial cell surface protein expression is unknown. Indirect evidence of endothelial cell molecular
heterogeneity comes from the reported ability of certain cells and peptide sequences to home to specific
tissues after intravenous injection23-25. Several receptors to angiogenic factors have been identified26-28 and
genomic analysis of endothelial cells isolated from tumours has provided angiogenic markers of unknown
subcellular localization29. Genetically induced endothelial cell targets provide 'proof of principle' that
immuno-targeting endothelium can cause tumour regression30; however, few probes to native endothelial cell
surface proteins show validated tissue-specific pharmacodelivery in vivo14, 15, 17, 24, 31, 32. This paucity of
molecular information may reflect the lack of tissue-induced proteins or, perhaps more likely, the difficulty
in studying such a minor cell type as it exists natively in the tissue without tissue disruption and isolation.
Although gene and immune targeting of tumour neovasculature seems promising33, 34, the ultimate potential of
endothelial targeting in creating new drug delivery systems remains unclear16, 17. The actual existence of
tissue-specific endothelial cell surface targets will remain uncertain until we overcome current technical
barriers to comprehensively map and validate tissue-induced endothelial cell surface proteins in vivo.
Molecular diversity of endothelium in vivo
To investigate endothelial cell surface heterogeneity in vivo, we performed subcellular fractionation to
isolate silica-coated luminal endothelial cell plasma membranes and their caveolae directly from normal
organs35, 36. These plasma membranes and their caveolae displayed a greater than 20-fold enrichment for
endothelial cell surface or caveolar markers (angiotensin converting enzyme (ACE), vascular endothelial
(VE)-cadherin and caveolin-1), whereas markers of intracellular organelles (for example, the Golgi protein
-COP), other tissue cells (for example, E-cadherin for epithelium, fibroblast surface protein) and blood (for
example, glycophorin A, CD4 and CD11) were greater than 20-fold depleted (Fig. 1c; data not shown and as shown
previously19, 35, 36). This quality control analysis was applied to each isolate.
Figure 1 Molecular heterogeneity of endothelial cell surface in multiple rat organs in vivo. Full legend
High resolution image and legend (78k)
We analysed these isolated plasma membranes by two-dimensional (2D) gel electrophoresis to produce
high-resolution vascular endothelial protein maps of the major rat organs, that were distinct and much reduced
in complexity from that of the starting tissue homogenate (Fig. 1a). Differential spot analysis detected many
distinct proteins in plasma membrane versus the homogenate and also in the plasma membrane between organs (Fig.
1b). Western blot analysis further confirmed this heterogeneity (Fig. 1c; data not shown). In many cases,
antigens difficult to detect in tissue homogenates were readily apparent in the isolated plasma membranes,
reflecting the significant enrichment and increased sensitivity provided by subfractionation to unmask proteins
located on the endothelial cell surface. Unique 'molecular fingerprints or signatures' that may include tissue-
and cell-specific proteins were apparent for each endothelium.
Subtractive analysis and profiling
To identify specific proteins expressed at the endothelial cell surface we used mass spectrometry, database
searching and immuno-blotting, to analyse endothelial plasma membranes and caveolae isolated from rat
tissues35, 36, as well as cultured rat lung microvascular endothelial cells (RLMVEC), isolated and grown in
culture37. So far, we have identified nearly 2,000 non-redundant proteins (our unpublished observation) which
were entered into a database (Accessible Vascular Targets, AVATAR) that was designed and annotated to provide
relational analysis between measurements and samples. To identify lung-induced, and possibly, lung-specific
endothelial cell surface proteins we used a systems biology approach, based on the hypothesis that the
surrounding tissue microenvironment (normal or diseased) modulates protein expression in the vascular
endothelium. We subtracted, in silico, the proteins identified in endothelial plasma membranes from rat lungs
versus RLMVEC because tissue-dependent protein expression may be reduced in cell culture that cannot yet
duplicate conditions in vivo. To increase certainty of expression in vivo versus in vitro, we applied a strict
identification criterion of 6 tandem mass spectrometry (MS/MS) spectra to rat lung endothelial plasma membranes
versus low stringency of 1 MS/MS spectra to RLMVEC plasma membranes. From the current rat database of
approximately 40,000 entries, we identified 37 differentially expressed proteins. To meet our objective of
direct exposure to circulating antibodies, we applied bioinformatic interrogation of structure, glycosylation
and membrane orientation to reduce the list to 11 proteins likely to have domains outside the cell.
To confirm the original mass spectrometry findings and to assess organ-specificity, we performed expression
profiling with specific antibodies. Consistent with our hypothesis, western blot analysis detected all 11
proteins enriched in lung endothelial plasma membranes (Fig. 1c) but not in RLMVEC plasma membranes (data not
shown). Each of these proteins exhibited a different pattern of restricted expression. Two proteins,
aminopeptidase P (APP) and OX-45, were detected only in endothelial plasma membranes from lung. Staining of
tissue sections with antibodies (including to APP and OX-45) confirmed this restricted expression (data not
shown). This profiling by western blot analysis was very sensitive and reliable, even at low expression levels.
Thus subtractive proteomic analysis provided a subset of endothelial cell proteins not expressed in vitro and
differentially expressed in vivo, apparently regulated by the unique tissue microenvironment in each organ.
Lung-specific targeting in vivo
To assess the immuno-accessibility of APP and OX-45 in vivo, including possible lung-specific targeting, we
intravenously injected 125I-labelled monoclonal antibodies into rats and performed whole-body imaging using
planar -scintigraphy. Within 20 min, we observed clear lung images, indicating rapid and specific targeting of
APP antibody to the lung (Fig. 2a, c). Region-of-interest and biodistribution analysis confirmed this
lung-specific targeting with 65% of the injected dose per gram of tissue accumulating in the lungs and less
than 2% injected dose per gram of tissue in other organs and blood. Consistent with the low blood levels, the
heart cavity was readily apparent (Fig. 2a, arrowhead). Furthermore, this lung targeting was inhibited by
addition of a 50-fold excess of unlabelled APP IgG but not with control IgG (data not shown), showing the
specific ability of our antibodies to bind APP exposed on the endothelial cell surface of the lung but not
other organs.
Figure 2 In vivo -scintigraphic imaging of APP antibody targeting in normal and tumour-bearing rats. Full
legend
High resolution image and legend (50k)
Consistent with OX-45 expression in various leukocytes38, we detected OX-45 (but not APP) in blood. Thus,
imaging with the OX-45 antibody showed little targeting to the lung (data not shown). Biodistribution analysis
confirmed only 2% of the injected dose per gram of tissue accumulating in the lung and greater than 70% of the
injected dose per gram of tissue remaining in the blood, primarily bound to the buffy coat subfraction of the
blood.
APP was reported to be expressed on mouse blood vessels of normal breast and mammary adenocarcinomas as a
target for a homing peptide39. High resolution single photon emission computed tomography (SPECT) imaging of
125I-APP antibodies injected intravenously into female rats detected no accumulation in normal breast tissue
(Fig. 2a) or in primary or metastatic breast tumour lesions (Fig. 2b; and multiple images taken over 36 hours
(data not shown)). SPECT imaging provided a clear three-dimensional view of normal lungs (Fig. 2c) which was in
striking contrast to the irregular images, with multiple nodular regions lacking signal, in rats with mammary
adenocarcinomas in the lung (Fig. 2d). Thus, based on the immuno-targeting imaged in vivo, endothelial APP
expression in the rat appeared quite specific for normal lung tissue, apparently induced by conditions present
in the normal lung tissue microenvironment, but absent in the tumour milieu in vivo, even when the tumour blood
vessels are derived from the normal lung vasculature.
Tumour-induced endothelial cell proteins
To determine whether the tumour microenvironment in the lung is sufficiently different to induce new
endothelial protein expression, we isolated silica-coated luminal endothelial cell plasma membranes and their
caveolae from normal rat lungs and lungs bearing breast adenocarcinomas35, 36 (Fig. 3a). As above, these
isolates were significantly enriched relative to the tissue homogenates in endothelial cell surface markers
(caveolin, 5' nucleotidase, ACE and VE-cadherin) and markedly depleted in markers of possible contaminants
(including -COP, CD4, CD11, glycophorin A, fibroblast surface protein and galectin-1, that is expressed by the
tumour cells40) (Fig. 3e and data not shown). The endothelial plasma membranes isolated from tumours expressed
multiple angiogenesis markers (enriched relative to both tumour homogenates and normal lung endothelial cell
plasma membranes). Lastly, markers of immune cells known to infiltrate solid tumours were detected in tumour
homogenates but not its endothelial cell plasma membranes.
Figure 3 Mapping rat lung tumours and organs for differential endothelial cell surface protein expression in
vivo. Full legend
High resolution image and legend (117k)
We used 2D gels to visualize several hundred protein spots in endothelial cell plasma membranes from normal
lungs versus tumours in lungs. These maps were reproducible (Fig. 3b). Multiple protein spots were detected in
these tumour but not normal endothelial plasma membranes (Fig. 3c). Prominent 2D spots easily detected in
tumour plasma membranes were not detected in the homogenates (Fig. 3d), consistent with the small percentage of
endothelial cell plasma membranes in the tumours. Tissue subfractionation appeared necessary to unmask
differentially expressed tumour vascular proteins obscured by the molecular complexity of the total tumour.
Again, we applied a subtractive proteomic approach using antibody and mass spectrometric analysis of these
plasma membranes and caveolae isolated from them to identify 15 differentially expressed proteins (Fig. 3e),
including proteins already implicated in tumour angiogenesis: vascular endothelial growth factor (VEGF)
receptors-1 and -2; Tie2; aminopeptidase-N; endoglin; carcinoembryonic antigen-related cell adhesion molecule 1
(CD66)' (C-CAM-1) and neuropilin-127, 28. These proteins were enriched in the tumour endothelial plasma
membranes relative to tumour homogenates, consistent with proper subfractionation. Eight new tumour-induced
vascular proteins were also identified: annexin A1; annexin A8; ephrin A5; ephrin A7; myeloperoxidase;
nucleolin; transferrin receptor and vitamin D-binding protein. Consistent with the subtractive screen
hypothesis, 12 out of 15 proteins were much more evident in tumour endothelial plasma membranes than in normal
plasma membranes.
Expression profiling using endothelial plasma membranes isolated from major organs demonstrated that almost all
of these proteins exist at the endothelial cell surface of at least one major organ, albeit mostly at levels
much less than tumours (Fig. 3e). One promising tumour candidate target was the 34 KDa protein recognized by
annexin A1 (AnnA1) antibodies only in tumour endothelial plasma membrane. Tissue immuno-histochemistry
confirmed tumour blood vessel reactivity (data not shown). Thus, the tumour microenvironment appeared to induce
distinct protein expression on the endothelial cell surface.
Targeting and imaging of solid tumours
Annexins are cytosolic proteins that can associate with cell membranes in a calcium-dependent manner41. Some
annexins may translocate the lipid bilayer to the external cell surface41. To test whether AnnA1 is
sufficiently exposed and tumour vessel specific to permit immuno-targeting in vivo, we performed whole-body
imaging using 125I-labelled AnnA1 monoclonal antibodies. -scintigraphic planar images captured four hours
postinjection showed a distinct focus of radioactivity in the lung and little signal elsewhere, in the bodies
of rats with tumours (Fig. 4a, b). Non-targeting 125I-labelled IgG did not show detectable selective tumour
uptake (data not shown). When the lungs were imaged ex vivo, we observed 125I-AnnA1 antibody accumulation in
the tumour as hot spots corresponding to visible tumours (Fig. 4c, d). Furthermore, targeting was prevented by
a 30-fold excess of unlabelled AnnA1 IgG but not by control IgG (data not shown). Region-of-interest and
biodistribution analysis confirmed targeting in vivo with an average tumour accumulation at two hours of 34%
injected dose per gram of tissue. This compared favourably to VEGF receptor antibodies which accumulated at
6.4% injected dose per gram of tumour. When injected into rats without tumours, 125I-AnnA1 antibodies showed no
targeting of normal organs, including lung at levels less than 1% injected dose per gram of tissue, whereas
VEGF receptor antibody accumulation was greater in multiple organs (data not shown). The uptake ratio in rat
tumour-bearing lungs versus normal lungs was up to 2.0 and 70 for antibodies to VEGF receptor and AnnA1,
respectively. Thus, -scintigraphic imaging rapidly validated AnnA1 as a tumour target that is readily
accessible to antibody injected intravenously for tumour targeting and imaging in vivo. AnnA1 appeared to be
selectively externalized on the endothelial cell surface in the solid tumours.
Figure 4 Tumour-specific targeting of 125I-AnnA1 antibodies after intravenous injection into tumour-bearing
rats. Full legend
High resolution image and legend (23k)
Radio-immunotherapy of solid tumours
Many tumour-bearing rats imaged with the 125I-AnnA1 antibody survived, so we performed a survival study and
recorded animal body weights; 80% of the animals treated with the 125I-AnnA1 antibody survived 8 days or longer
compared with the 125I-IgG-treated and untreated rats, which died within 7 days (Fig. 5a). The body weights of
all tumour-bearing rats began to drop 7–10 days after tumour cell inoculation (Fig. 5b). The control rats
continued to decrease in body weight to 23–30% less than normal at their death. In contrast, rats treated with
125I-AnnA1 IgG began to gain weight within 3–4 days and reached a normal body weight after 25 days. This
increased survival was striking because in this model many animals die within 2–4 days of treatment and thus
may lack sufficient time to benefit from treatment. The survival rate of rats surviving the first week
approached 90%. The one rat that died after 2 weeks required euthanasia because of a leg tumour and large tail
tumour that were not apparent when treated. Thus, a single injection of 125I-AnnA1 antibody caused significant
remission even in advanced disease.
Figure 5 AnnA1 targeted radio-immunotherapy increases survival in rats. Full legend
High resolution image and legend (22k)
AnnA1 in human tumour neovasculature
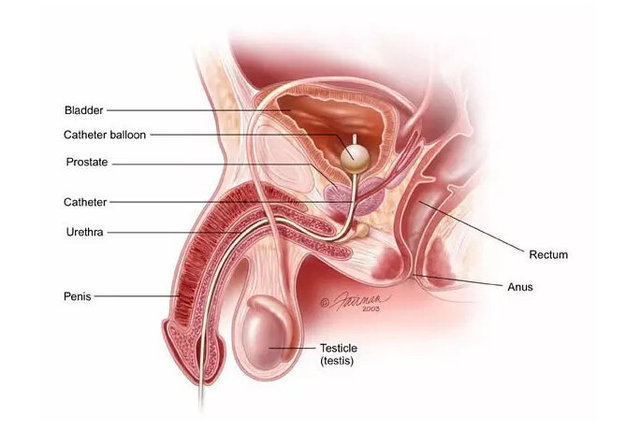
We immuno-stained tissue sections of human solid tumours. AnnA1 antibody labelled blood vessels of human
prostate, liver, breast and lung tumours but not matched normal tissues (Fig. 6). Antibodies to platelet
endothelial cell adhesion molecule-1 (PECAM) stained both normal and tumour blood vessels. The lack of AnnA1
expression in vascular endothelium of multiple normal organs has been reported previously42-45. Thus, AnnA1 was
selectively detected on the neovascular endothelium of multiple human solid tumours.
Figure 6 Expression of AnnA1 on vascular endothelium of multiple primary human solid tumours. Full legend
High resolution image and legend (99k)
Discussion
We describe a new logic-based discovery and validation approach that integrates newly developed, global
analytical techniques to map the proteins expressed in vivo at the luminal endothelial cell surface. This
approach has demonstrated distinct molecular signatures in normal and neoplastic tissues. We applied this
strategy to rat lungs and solid tumours to uncover, from the vast number of proteins expressed in tissue,
approximately 50 differentially expressed proteins, including two promising tissue-selective endothelial cell
surface proteins that permitted rapid and specific immuno-targeting and imaging in vivo. Profiling the
endothelial cell surface that is accessible in vivo is an important logical step for validating the hypothesis
of tissue-modulated endothelial cell diversity in vivo and for discovering potential targets. This is important
not only to direct pharmacodelivery and molecular imaging but also—by means of caveolae—to overcome the
restrictive endothelial cell barrier to transport drugs or genes to the underlying tissue cells16, 17.
Key features of our analysis included tissue subfractionation with subtractive proteomic and bioinformatic
filters that together reduced tissue complexity by greater than five orders of magnitude, and unmasked a
manageable subset of proteins at the inherently accessible blood–tissue interface. This has led to the
creation of a database of vascular endothelial cell surface proteins containing accessible proteins apparently
modulated by the tissue. After bioinformatic filtering, western blot analysis and/or tissue immuno-staining
provided sensitive expression profiling to yield only a few candidate proteins exhibiting organ- or
tumour-specificity. Planar and SPECT imaging, using intravenously injected antibodies specific to each protein,
visualized targeting and tissue accumulation with high sensitivity and resolution. Imaging thus provided a
rigorous and objective validation of accessibility and tissue-specificity of the few remaining candidate
targets and ultimately demonstrated potential utility such as, how rapidly and to what extent the antibody
targets single organs or solid tumours in vivo.
So far, in vivo imaging correlates well with the expression profiling using isolated endothelial plasma
membranes. It showed lung-specific immuno-targeting for APP (Fig. 2), tumour-specificity for AnnA1 (Fig. 4) and
targeting of multiple tissues for less specific target proteins (that is, PV-1, VEGF-R and podocalyxin) (our
unpublished observations). Because of poor access inside many tissues, antibodies injected intravenously
usually require significantly higher doses (250 µg kg-1 (ref. 46) compared with 20 µg kg-1 used here) to get a
small percentage into the tissue that binds and can then be visualized clearly a day or so later, after the
background signal has been cleared from the blood. Here, the binding was direct and unhindered by barriers so
that both tissue accumulation and blood clearance were rapid, thereby providing striking images within minutes
to hours. The rapidity and high levels of specific targeting observed here meet the theoretical expectation of
the vascular targeting strategy17. Although fast emerging as a standard for assessing targeting and
specificity1-4, whole-body imaging may be underutilized in target validation despite being non-invasive and
highly sensitive.
Using a new, integrated analytical approach we have found new tissue-specific endothelial cell surface proteins
that can act as vascular targets to bring us one step closer to achieving the century-old elusive goal of
targeting single organs or solid tumours in vivo1, 2, 4, 6, 10. The development and optimization of several key
technologies has provided the sensitivity and throughput required for this new target discovery and validation
process. We expect that site-directed vascular and caveolar targeting will benefit both drug and gene delivery
in the treatment of many diseases16. We have demonstrated here, using a rat tumour model that monoclonal
antibodies to AnnA1 can effectively direct low levels of radionuclides (100 µCi) to concentrate in, and thus
destroy solid tumours, which ultimately increases animal survival. Because AnnA1 is also selectively detected
in multiple human solid tumours, this target may similarly help to image and treat human disease.
Methods
A detailed description of the materials, 2D gel analysis, expression profiling in vivo of candidate proteins,
rat tumour models, -scintigraphic imaging and biodistribution analysis is available in Supplementary Methods.
Proteomic analysis We used a three-pronged approach to resolve proteins/peptides for mass spectrometric
analysis: (1) The proteins of silica-coated luminal endothelial cell plasma membranes and caveolae isolated
from various normal organs or tumours were resolved by high resolution 2D gel analysis before excising
potential organ- or tumour-specific protein spots for mass spectrometric analysis; (2) Proteins in the isolated
endothelial plasma membranes and caveolae were separated using one-dimensional (1D) SDS–polyacrylamide gel
electrophoresis (SDS–PAGE) and specific bands of interest were cut out or the whole gel lane was cut into 50
slices, and the proteins in each of the gel slices were analysed by mass spectrometry; and (3)
Multi-dimensional Protein Identification Technology (MudPIT) was used to analyse tryptic peptides from a
complex mixture of proteins extracted directly from the whole isolated endothelial plasma membrane fraction and
caveolae isolates. Each gel spot/slice was de-stained and digested overnight with trypsin before extracting the
cleaved peptides from the gel and then loading them onto a reverse phase micro-column for gradient acetonitrile
elution directly into the mass spectrometer (LCQ Deca XP ion trap mass spectrometer (ThermoFinnigan) equipped
with a modified micro-electrospray ionization source from Mass Evolution). For MudPIT, 150 µg of complex
peptide mixture was separated by 2D liquid chromatography, comprising a micro-column packed with three phases
of chromatographic material as follows: 8.5 cm of 5 µm reversed phase material (Polaris C18-A, Metachem); 4 cm
of 5 µm 300 Å strong cation exchanger (PolyLC); and lastly 3.5 cm of C18 material, using a helium pressure cell
operated at 600–900 psi (Mass Evolution). Peptides were directly eluted into the mass spectrometer using 2D
chromatography with 18 step-elutions from the strong cation exchanger, followed by a gradient elution of the
reversed phase material. Operation of the quarternary Agilent 1100 HPLC pump and the mass spectrometer was
fully automated during the entire procedure using the Excalibur 1.2 data system (ThermoFinnigan). Continuous
cycles of one full scan (m/z 400 to 1,400) followed by three data-dependent MS/MS measurements at 35%
normalized collision energy were performed. MS/MS measurements were allowed for the three most intense
precursor ions with an enabled exclusion list of 25 m/z values ( 1.5 Da) or a maximum time limit of 5 min. The
zoom scan function to determine the charge state was disabled in order to increase the duty cycle of the
instrument.
Database search and in silico analysis of tandem mass spectra MS/MS spectra were extracted from raw files
requiring a minimum of 21 signals with an intensity of at least 4.75 104 arbitrary units (AU). Extracted MS/MS
spectra were automatically assigned to the best matching peptide sequence using the SEQUEST algorithm and the
Sequest Browser software package (ThermoFinnigan). SEQUEST searches were performed using a rat protein database
containing 40,800 protein sequences that were downloaded as FASTA formatted sequences from ENTREZ (National
Center for Biotechnology Information (NCBI); http://www.ncbi.nlm.nih.gov/Entrez). Sequence redundancies were
removed using Perl script. The peptide mass search tolerance was set to 3 Da. Spectral matches were retained
with a minimal cross-correlation score (XCorr) of 1.5, 2.2 and 3.3 for charge states +1, +2 and +3,
respectively. DeltaCN (top match's XCorr minus the second-best match's XCorr, divided by top match's XCorr) had
to be equal or less than 0.07. Retained spectral matches were filtered and re-assigned to proteins using
DTASelect. DTASelect outputs of independent measurements were entered into the AVATAR database. AVATAR was
designed to store a large amount of mass spectrometric data and to provide tools to analyse the data to extract
valuable information. We used relational models for database design based on entity relationship and
implemented the database in the MySQL relational database management system (MySQL) to support database query
and management. This relational database plus the Perl-based interface greatly improved data organization, data
consistency and integrity, and facilitated data comparison and information retrieval. In the case of the 1D gel
and MudPIT approaches, AVATAR was used to subtract the data to find proteins detected only at the lung
endothelial cell surface in vivo versus in vitro or on the tumour but not normal endothelium.
In silico bioinformatic interrogation To identify possible candidates for intravenously accessible targets from
the subset of proteins identified as lung or tumour induced, we determined their currently known
membrane-associated structure (bilayer spanning versus lipid anchor (intra- or extracellular) versus peripheral
interaction) from scientific reports and/or protein databases, such as SwissProt
(http://us.expasy.org/sprot/sprot-top.html) and the NCBI ENTREZ protein database
(http://www.ncbi.nlm.nih.gov/entrez/query.fcgi). We also used web-based prediction programs to identify
candidates that may harbour transmembrane spanning alpha helices (Prediction of Transmembrane Regions and
Orientation (TMpred), http://www.ch.embnet.org/software/TMPRED_form.html) or glycosylation sites to indicate a
possible ectodomain exposed to the circulating blood (Prosite Scan,
http://npsa-pbil.ibcp.fr/cgi-bin/npsa_automat.pl?page = npsa_prosite.html). Only 100% probabilities were taken
into consideration.
Supplementary information accompanies this paper.
Received 28 January 2004;accepted 19 April 2004
References 1. Massoud, T. F. & Gambhir, S. S. Molecular imaging in living subjects: seeing fundamental
biological processes in a new light. Genes Dev. 17, 545–580 (2003) | Article | PubMed | ISI | ChemPort |
2. Herschman, H. R. Molecular imaging: looking at problems, seeing solutions. Science 302, 605–608 (2003) |
Article | PubMed | ISI | ChemPort |
3. Rudin, M. & Weissleder, R. Molecular imaging in drug discovery and development. Nature Rev. Drug Discov. 2,
123–131 (2003) | Article | PubMed | ISI | ChemPort |
4. Weissleder, R. Scaling down imaging: molecular mapping of cancer in mice. Nature Rev. Cancer 2, 11–18
(2002) | Article | PubMed | ISI | ChemPort |
5. Drews, J. Drug discovery: a historical perspective. Science 287, 1960–1964 (2000) | Article | PubMed | ISI
| ChemPort |
6. Lindsay, M. A. Target discovery. Nature Rev. Drug Discov. 2, 831–838 (2003) | Article | PubMed | ISI |
ChemPort |
7. Workman, P. New drug targets for genomic cancer therapy: successes, limitations, opportunities and future
challenges. Curr. Cancer Drug Targets 1, 33–47 (2001) | PubMed | ChemPort |
8. Anzick, S. L. & Trent, J. M. Role of genomics in identifying new targets for cancer therapy. Oncology
(Huntingt.) 16, 7–13 (2002) | PubMed |
9. Cavenee, W. K. Genetics and new approaches to cancer therapy. Carcinogenesis 23, 683–686 (2002) | Article |
PubMed | ISI | ChemPort |
10. Huber, L. A. Is proteomics heading in the wrong direction? Nature Rev. Mol. Cell Biol. 4, 74–80 (2003) |
Article | PubMed | ISI | ChemPort |
11. Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752 (2000) | Article |
PubMed | ISI | ChemPort |
12. Jain, R. K. The next frontier of molecular medicine: delivery of therapeutics. Nature Med. 4, 655–657
(1998) | Article | PubMed | ISI | ChemPort |
13. Dvorak, H. F., Nagy, J. A. & Dvorak, A. M. Structure of solid tumors and their vasculature: implications
for therapy with monoclonal antibodies. Cancer Cells 3, 77–85 (1991) | PubMed | ISI | ChemPort |
14. von Mehren, M., Adams, G. P. & Weiner, L. M. Monoclonal antibody therapy for cancer. Annu. Rev. Med. 54,
343–369 (2003) | Article | PubMed | ISI | ChemPort |
15. Farah, R. A., Clinchy, B., Herrera, L. & Vitetta, E. S. The development of monoclonal antibodies for the
therapy of cancer. Crit. Rev. Eukaryot. Gene Expr. 8, 321–356 (1998) | PubMed | ISI | ChemPort |
16. Carver, L. A. & Schnitzer, J. E. Caveolae: mining little caves for new cancer targets. Nature Rev. Cancer
3, 571–581 (2003) | Article | PubMed | ISI | ChemPort |
17. Schnitzer, J. E. Vascular targeting as a strategy for cancer therapy. N. Engl. J. Med. 339, 472–474 (1998)
| Article | PubMed | ISI | ChemPort |
18. Madri, J. A. & Williams, S. K. Capillary endothelial cell culture: Phenotype modulation by matrix
components. J. Cell Biol. 97, 153–165 (1983) | Article | PubMed | ISI | ChemPort |
19. Schnitzer, J. E. in Vascular Endothelium: Physiology, Pathology and Therapeutic Opportunities (eds Born, G.
V. R. & Schwartz, C. J.) 77–95 (Schattauer, Stuttgart, 1997)
20. Aird, W. C. et al. Vascular bed-specific expression of an endothelial cell gene is programmed by the tissue
microenvironment. J. Cell Biol. 138, 1117–1124 (1997) | Article | PubMed | ISI | ChemPort |
21. Janzer, R. C. & Raff, M. C. Astrocytes induce blood–brain barrier properties in endothelial cells. Nature
325, 253–257 (1987) | Article | PubMed | ISI | ChemPort |
22. Stewart, P. A. & Wiley, M. J. Developing nervous tissue induces formation of blood-brain barrier
characteristics in invading endothelial cells: a study using quail-chick transplantation chimeras. Dev. Biol.
84, 183–192 (1981) | PubMed | ISI | ChemPort |
23. Auerbach, R. et al. Specificity of adhesion between murine tumor cells and capillary endothelium: an in
vitro correlate of preferential metastasis in vivo. Cancer Res. 47, 1492–1496 (1987) | PubMed | ISI | ChemPort
|
24. Pasqualini, R. & Ruoslahti, E. Organ targeting in vivo using phage display peptide libraries. Nature 380,
364–366 (1996) | Article | PubMed | ISI | ChemPort |
25. Rajotte, D. et al. Molecular heterogeneity of the vascular endothelium revealed by in vivo phage display.
J. Clin. Invest. 102, 430–437 (1998) | PubMed | ISI | ChemPort |
26. Papetti, M. & Herman, I. M. Mechanisms of normal and tumor-derived angiogenesis. Am. J. Physiol. Cell
Physiol. 282, C947–C970 (2002) | PubMed | ISI | ChemPort |
27. Ferrara, N. VEGF and the quest for tumour angiogenesis factors. Nature Rev. Cancer 2, 795–803 (2002) |
Article | PubMed | ISI | ChemPort |
28. Kerbel, R. & Folkman, J. Clinical translation of angiogenesis inhibitors. Nature Rev. Cancer 2, 727–739
(2002) | Article | PubMed | ISI | ChemPort |
29. St Croix, B. et al. Genes expressed in human tumor endothelium. Science 289, 1197–1202 (2000) | Article |
PubMed | ISI | ChemPort |
30. Huang, X. et al. Tumor infarction in mice by antibody-directed targeting of tissue factor to tumor
vasculature. Science 275, 547–550 (1997) | Article | PubMed | ISI | ChemPort |
31. McIntosh, D. P., Tan, X.-Y., Oh, P. & Schnitzer, J. E. Targeting endothelium and its dynamic caveolae for
tissue-specific transcytosis in vivo: A pathway to overcome cell barriers to drug and gene delivery. Proc. Natl
Acad. Sci. USA 99, 1996–2001 (2002) | Article | PubMed | ChemPort |
32. Sipkins, D. A. et al. Detection of tumor angiogenesis in vivo by alphaVbeta3-targeted magnetic resonance
imaging. Nature Med. 4, 623–626 (1998) | Article | PubMed | ISI | ChemPort |
33. Hu, Z. & Garen, A. Targeting tissue factor on tumor vascular endothelial cells and tumor cells for
immunotherapy in mouse models of prostatic cancer. Proc. Natl Acad. Sci. USA 98, 12180–12185 (2001) | Article
| PubMed | ChemPort |
34. Hood, J. D. et al. Tumor regression by targeted gene delivery to the neovasculature. Science 296, 2404–
2407 (2002) | Article | PubMed | ISI | ChemPort |
35. Oh, P. & Schnitzer, J. E. in Cell Biology: A Laboratory Handbook (ed. Celis, J.) 34–36 (Academic Press,
Orlando, 1998)
36. Schnitzer, J. E., McIntosh, D. P., Dvorak, A. M., Liu, J. & Oh, P. Separation of caveolae from associated
microdomains of GPI-anchored proteins. Science 269, 1435–1439 (1995) | PubMed | ISI | ChemPort |
37. Schnitzer, J. E. gp60 is an albumin-binding glycoprotein expressed by continuous endothelium involved in
albumin transcytosis. Am. J. Physiol. 262, H246–H254 (1992) | PubMed | ISI | ChemPort |
38. Henniker, A. J., Bradstock, K. F., Grimsley, P. & Atkinson, M. K. A novel non-lineage antigen on human
leucocytes: characterization with two CD-48 monoclonal antibodies. Dis. Markers 8, 179–190 (1990) | PubMed |
ISI | ChemPort |
39. Essler, M. & Ruoslahti, E. Molecular specialization of breast vasculature: a breast-homing phage-displayed
peptide binds to aminopeptidase P in breast vasculature. Proc. Natl Acad. Sci. USA 99, 2252–2257 (2002) |
Article | PubMed | ChemPort |
40. Perillo, N. L., Marcus, M. E. & Baum, L. G. Galectins: versatile modulators of cell adhesion, cell
proliferation, and cell death. J. Mol. Med. 76, 402–412 (1998) | Article | PubMed | ISI | ChemPort |
41. Gerke, V. & Moss, S. E. Annexins: from structure to function. Physiol. Rev. 82, 331–371 (2002) | PubMed |
ISI | ChemPort |
42. Dreier, R., Schmid, K. W., Gerke, V. & Riehemann, K. Differential expression of annexins I, II and IV in
human tissues: an immunohistochemical study. Histochem. Cell Biol. 110, 137–148 (1998) | Article | PubMed |
ISI | ChemPort |
43. Eberhard, D. A., Brown, M. D. & VandenBerg, S. R. Alterations of annexin expression in pathological
neuronal and glial reactions. Immunohistochemical localization of annexins I, II (p36 and p11 subunits), IV,
and VI in the human hippocampus. Am. J. Pathol. 145, 640–649 (1994) | PubMed | ISI | ChemPort |
44. Ahn, S. H., Sawada, H., Ro, J. Y. & Nicolson, G. L. Differential expression of annexin I in human mammary
ductal epithelial cells in normal and benign and malignant breast tissues. Clin. Exp. Metastasis 15, 151–156
(1997) | Article | PubMed | ISI | ChemPort |
45. McKanna, J. A. & Zhang, M. Z. Immunohistochemical localization of lipocortin 1 in rat brain is sensitive to
pH, freezing, and dehydration. J. Histochem. Cytochem. 45, 527–538 (1997) | PubMed | ISI | ChemPort |
46. Bredow, S., Lewin, M., Hofmann, B., Marecos, E. & Weissleder, R. Imaging of tumour neovasculature by
targeting the TGF-beta binding receptor endoglin. Eur. J. Cancer 36, 675–681 (2000) | Article | PubMed | ISI |
ChemPort |
Acknowledgements. We thank A. Wempren, K. Hearn, M. Bourne, L. Randall and T. Smith for technical assistance.
This research was supported by the National Institute of Health (Heart, Lung and Blood), National Cancer
Institute, Sidney Kimmel, Schutz Foundation, California Tobacco-related Disease Research Program and California
Breast Cancer Research Program.
Competing interests statement. The authors declare that they have no competing financial interests
按:蛋白质组学的技术可以是我们鉴定大量的差异蛋白,但是这也给进一步确证工作带来了巨大的压力。蛋白质组学不仅要做
到多,还应该进一步做到少。这种由少到多再到少,是一个升华。
一个清晰的轮廓,这使得蛋白质组学在药物靶点寻找方面还停留在概念上。而最近Nature上的一篇文章是我们看到一线曙光。
Sidney Kimmel癌症研究中心的SCHNITZER 领导的研究小组采用削减蛋白质组作图的方法加快蛋白组学寻找药物靶点的工作。
Nature 429, 629 - 635
PHIL OH, YAN LI, JINGYI YU, EBERHARD DURR, KAROLINA M. KRASINSKA, LUCY A. CARVER, JACQUELINE E. TESTA & JAN E.
SCHNITZER
Sidney Kimmel Cancer Center, 10835 Altman Row, San Diego, California 92121, USA
Correspondence and requests for materials should be addressed to J.E.S. (jschnitzer@skcc.org).
Subtractive proteomic mapping of the endothelial surface in lung and solid tumours for tissue-specific therapy
The molecular complexity of tissues and the inaccessibility of most cells within a tissue limit the discovery
of key targets for tissue-specific delivery of therapeutic and imaging agents in vivo. Here, we describe a
hypothesis-driven, systems biology approach to identifying a small subset of proteins induced at the tissue–
blood interface that are inherently accessible to antibodies injected intravenously. We use subcellular
fractionation, subtractive proteomics and bioinformatics to identify endothelial cell surface proteins
exhibiting restricted tissue distribution and apparent tissue modulation. Expression profiling and
-scintigraphic imaging with antibodies establishes two of these proteins, aminopeptidase-P and annexin A1, as
selective in vivo targets for antibodies in lungs and solid tumours, respectively. Radio-immunotherapy to
annexin A1 destroys tumours and increases animal survival. This analytical strategy can map tissue- and
disease-specific expression of endothelial cell surface proteins to uncover novel accessible targets useful for
imaging and therapy.
New targets are needed for detecting disease through molecular imaging1-4 and for treating disease through
directed delivery in vivo5-9. Sequencing the human genome has identified a target pool of 40,000 genes which
may translate into a million possible protein targets10. Genomic and proteomic analysis of normal and diseased
tissues has yielded thousands of genes and gene products for diagnostic and tissue assignment as well as
potential therapeutic targets5-11. But the shear number of candidates can overwhelm the required in vivo
validation process, leading some to question the ultimate impact of these approaches on speeding up drug
discovery5-7, 10. Reducing tissue data complexity to a manageable subset of candidates most relevant to
targeting, imaging and treating disease is clearly desired but requires new discovery and validation
strategies, that effectively focus the power of global identification technologies.
Selectively targeting a single organ or diseased tissue (such as a solid tumour) in vivo remains a desirable
but elusive goal for molecular medicine12, 13. This targeting would allow more effective imaging as well as
drug and gene therapies for many acquired and genetic diseases1-4, 6, 7, 10-13. Most tissue- and
disease-associated proteins are expressed by cells inside tissue compartments not readily accessible to
intravenously injected biological agents such as antibodies. This inaccessibility hinders many site-directed
therapies5-7, 12, 13 and imaging agents1-4. For example, multiple barriers to delivery prevent effective
immunotherapy for solid tumours in vivo, despite efficacy and specificity in vitro12-17. Conversely, the nearly
universal access of chemotherapeutics dilutes efficacy requiring increased dosages, leading to unwanted
systemic side effects. Thus, new approaches are required to filter the overabundance of molecular information
to allow rapid discovery and validation of accessible tissue-specific targets that can direct molecular imaging
and pharmacodelivery in vivo.
Here, we divert analytical focus from the poorly accessible cells inside tissues to the critical tissue–blood
interface, inherently accessible to agents absorbed or injected into the blood. The endothelium is a minor
tissue component that exists as an attenuated cell monolayer lining all blood vessels and is in direct contact
with the circulating blood. The tissue microenvironment surrounding blood vessels seems to control the
endothelial cell phenotype in vivo18-22. But the degree to which normal and diseased tissues can modulate
endothelial cell surface protein expression is unknown. Indirect evidence of endothelial cell molecular
heterogeneity comes from the reported ability of certain cells and peptide sequences to home to specific
tissues after intravenous injection23-25. Several receptors to angiogenic factors have been identified26-28 and
genomic analysis of endothelial cells isolated from tumours has provided angiogenic markers of unknown
subcellular localization29. Genetically induced endothelial cell targets provide 'proof of principle' that
immuno-targeting endothelium can cause tumour regression30; however, few probes to native endothelial cell
surface proteins show validated tissue-specific pharmacodelivery in vivo14, 15, 17, 24, 31, 32. This paucity of
molecular information may reflect the lack of tissue-induced proteins or, perhaps more likely, the difficulty
in studying such a minor cell type as it exists natively in the tissue without tissue disruption and isolation.
Although gene and immune targeting of tumour neovasculature seems promising33, 34, the ultimate potential of
endothelial targeting in creating new drug delivery systems remains unclear16, 17. The actual existence of
tissue-specific endothelial cell surface targets will remain uncertain until we overcome current technical
barriers to comprehensively map and validate tissue-induced endothelial cell surface proteins in vivo.
Molecular diversity of endothelium in vivo
To investigate endothelial cell surface heterogeneity in vivo, we performed subcellular fractionation to
isolate silica-coated luminal endothelial cell plasma membranes and their caveolae directly from normal
organs35, 36. These plasma membranes and their caveolae displayed a greater than 20-fold enrichment for
endothelial cell surface or caveolar markers (angiotensin converting enzyme (ACE), vascular endothelial
(VE)-cadherin and caveolin-1), whereas markers of intracellular organelles (for example, the Golgi protein
-COP), other tissue cells (for example, E-cadherin for epithelium, fibroblast surface protein) and blood (for
example, glycophorin A, CD4 and CD11) were greater than 20-fold depleted (Fig. 1c; data not shown and as shown
previously19, 35, 36). This quality control analysis was applied to each isolate.
Figure 1 Molecular heterogeneity of endothelial cell surface in multiple rat organs in vivo. Full legend
High resolution image and legend (78k)
We analysed these isolated plasma membranes by two-dimensional (2D) gel electrophoresis to produce
high-resolution vascular endothelial protein maps of the major rat organs, that were distinct and much reduced
in complexity from that of the starting tissue homogenate (Fig. 1a). Differential spot analysis detected many
distinct proteins in plasma membrane versus the homogenate and also in the plasma membrane between organs (Fig.
1b). Western blot analysis further confirmed this heterogeneity (Fig. 1c; data not shown). In many cases,
antigens difficult to detect in tissue homogenates were readily apparent in the isolated plasma membranes,
reflecting the significant enrichment and increased sensitivity provided by subfractionation to unmask proteins
located on the endothelial cell surface. Unique 'molecular fingerprints or signatures' that may include tissue-
and cell-specific proteins were apparent for each endothelium.
Subtractive analysis and profiling
To identify specific proteins expressed at the endothelial cell surface we used mass spectrometry, database
searching and immuno-blotting, to analyse endothelial plasma membranes and caveolae isolated from rat
tissues35, 36, as well as cultured rat lung microvascular endothelial cells (RLMVEC), isolated and grown in
culture37. So far, we have identified nearly 2,000 non-redundant proteins (our unpublished observation) which
were entered into a database (Accessible Vascular Targets, AVATAR) that was designed and annotated to provide
relational analysis between measurements and samples. To identify lung-induced, and possibly, lung-specific
endothelial cell surface proteins we used a systems biology approach, based on the hypothesis that the
surrounding tissue microenvironment (normal or diseased) modulates protein expression in the vascular
endothelium. We subtracted, in silico, the proteins identified in endothelial plasma membranes from rat lungs
versus RLMVEC because tissue-dependent protein expression may be reduced in cell culture that cannot yet
duplicate conditions in vivo. To increase certainty of expression in vivo versus in vitro, we applied a strict
identification criterion of 6 tandem mass spectrometry (MS/MS) spectra to rat lung endothelial plasma membranes
versus low stringency of 1 MS/MS spectra to RLMVEC plasma membranes. From the current rat database of
approximately 40,000 entries, we identified 37 differentially expressed proteins. To meet our objective of
direct exposure to circulating antibodies, we applied bioinformatic interrogation of structure, glycosylation
and membrane orientation to reduce the list to 11 proteins likely to have domains outside the cell.
To confirm the original mass spectrometry findings and to assess organ-specificity, we performed expression
profiling with specific antibodies. Consistent with our hypothesis, western blot analysis detected all 11
proteins enriched in lung endothelial plasma membranes (Fig. 1c) but not in RLMVEC plasma membranes (data not
shown). Each of these proteins exhibited a different pattern of restricted expression. Two proteins,
aminopeptidase P (APP) and OX-45, were detected only in endothelial plasma membranes from lung. Staining of
tissue sections with antibodies (including to APP and OX-45) confirmed this restricted expression (data not
shown). This profiling by western blot analysis was very sensitive and reliable, even at low expression levels.
Thus subtractive proteomic analysis provided a subset of endothelial cell proteins not expressed in vitro and
differentially expressed in vivo, apparently regulated by the unique tissue microenvironment in each organ.
Lung-specific targeting in vivo
To assess the immuno-accessibility of APP and OX-45 in vivo, including possible lung-specific targeting, we
intravenously injected 125I-labelled monoclonal antibodies into rats and performed whole-body imaging using
planar -scintigraphy. Within 20 min, we observed clear lung images, indicating rapid and specific targeting of
APP antibody to the lung (Fig. 2a, c). Region-of-interest and biodistribution analysis confirmed this
lung-specific targeting with 65% of the injected dose per gram of tissue accumulating in the lungs and less
than 2% injected dose per gram of tissue in other organs and blood. Consistent with the low blood levels, the
heart cavity was readily apparent (Fig. 2a, arrowhead). Furthermore, this lung targeting was inhibited by
addition of a 50-fold excess of unlabelled APP IgG but not with control IgG (data not shown), showing the
specific ability of our antibodies to bind APP exposed on the endothelial cell surface of the lung but not
other organs.
Figure 2 In vivo -scintigraphic imaging of APP antibody targeting in normal and tumour-bearing rats. Full
legend
High resolution image and legend (50k)
Consistent with OX-45 expression in various leukocytes38, we detected OX-45 (but not APP) in blood. Thus,
imaging with the OX-45 antibody showed little targeting to the lung (data not shown). Biodistribution analysis
confirmed only 2% of the injected dose per gram of tissue accumulating in the lung and greater than 70% of the
injected dose per gram of tissue remaining in the blood, primarily bound to the buffy coat subfraction of the
blood.
APP was reported to be expressed on mouse blood vessels of normal breast and mammary adenocarcinomas as a
target for a homing peptide39. High resolution single photon emission computed tomography (SPECT) imaging of
125I-APP antibodies injected intravenously into female rats detected no accumulation in normal breast tissue
(Fig. 2a) or in primary or metastatic breast tumour lesions (Fig. 2b; and multiple images taken over 36 hours
(data not shown)). SPECT imaging provided a clear three-dimensional view of normal lungs (Fig. 2c) which was in
striking contrast to the irregular images, with multiple nodular regions lacking signal, in rats with mammary
adenocarcinomas in the lung (Fig. 2d). Thus, based on the immuno-targeting imaged in vivo, endothelial APP
expression in the rat appeared quite specific for normal lung tissue, apparently induced by conditions present
in the normal lung tissue microenvironment, but absent in the tumour milieu in vivo, even when the tumour blood
vessels are derived from the normal lung vasculature.
Tumour-induced endothelial cell proteins
To determine whether the tumour microenvironment in the lung is sufficiently different to induce new
endothelial protein expression, we isolated silica-coated luminal endothelial cell plasma membranes and their
caveolae from normal rat lungs and lungs bearing breast adenocarcinomas35, 36 (Fig. 3a). As above, these
isolates were significantly enriched relative to the tissue homogenates in endothelial cell surface markers
(caveolin, 5' nucleotidase, ACE and VE-cadherin) and markedly depleted in markers of possible contaminants
(including -COP, CD4, CD11, glycophorin A, fibroblast surface protein and galectin-1, that is expressed by the
tumour cells40) (Fig. 3e and data not shown). The endothelial plasma membranes isolated from tumours expressed
multiple angiogenesis markers (enriched relative to both tumour homogenates and normal lung endothelial cell
plasma membranes). Lastly, markers of immune cells known to infiltrate solid tumours were detected in tumour
homogenates but not its endothelial cell plasma membranes.
Figure 3 Mapping rat lung tumours and organs for differential endothelial cell surface protein expression in
vivo. Full legend
High resolution image and legend (117k)
We used 2D gels to visualize several hundred protein spots in endothelial cell plasma membranes from normal
lungs versus tumours in lungs. These maps were reproducible (Fig. 3b). Multiple protein spots were detected in
these tumour but not normal endothelial plasma membranes (Fig. 3c). Prominent 2D spots easily detected in
tumour plasma membranes were not detected in the homogenates (Fig. 3d), consistent with the small percentage of
endothelial cell plasma membranes in the tumours. Tissue subfractionation appeared necessary to unmask
differentially expressed tumour vascular proteins obscured by the molecular complexity of the total tumour.
Again, we applied a subtractive proteomic approach using antibody and mass spectrometric analysis of these
plasma membranes and caveolae isolated from them to identify 15 differentially expressed proteins (Fig. 3e),
including proteins already implicated in tumour angiogenesis: vascular endothelial growth factor (VEGF)
receptors-1 and -2; Tie2; aminopeptidase-N; endoglin; carcinoembryonic antigen-related cell adhesion molecule 1
(CD66)' (C-CAM-1) and neuropilin-127, 28. These proteins were enriched in the tumour endothelial plasma
membranes relative to tumour homogenates, consistent with proper subfractionation. Eight new tumour-induced
vascular proteins were also identified: annexin A1; annexin A8; ephrin A5; ephrin A7; myeloperoxidase;
nucleolin; transferrin receptor and vitamin D-binding protein. Consistent with the subtractive screen
hypothesis, 12 out of 15 proteins were much more evident in tumour endothelial plasma membranes than in normal
plasma membranes.
Expression profiling using endothelial plasma membranes isolated from major organs demonstrated that almost all
of these proteins exist at the endothelial cell surface of at least one major organ, albeit mostly at levels
much less than tumours (Fig. 3e). One promising tumour candidate target was the 34 KDa protein recognized by
annexin A1 (AnnA1) antibodies only in tumour endothelial plasma membrane. Tissue immuno-histochemistry
confirmed tumour blood vessel reactivity (data not shown). Thus, the tumour microenvironment appeared to induce
distinct protein expression on the endothelial cell surface.
Targeting and imaging of solid tumours
Annexins are cytosolic proteins that can associate with cell membranes in a calcium-dependent manner41. Some
annexins may translocate the lipid bilayer to the external cell surface41. To test whether AnnA1 is
sufficiently exposed and tumour vessel specific to permit immuno-targeting in vivo, we performed whole-body
imaging using 125I-labelled AnnA1 monoclonal antibodies. -scintigraphic planar images captured four hours
postinjection showed a distinct focus of radioactivity in the lung and little signal elsewhere, in the bodies
of rats with tumours (Fig. 4a, b). Non-targeting 125I-labelled IgG did not show detectable selective tumour
uptake (data not shown). When the lungs were imaged ex vivo, we observed 125I-AnnA1 antibody accumulation in
the tumour as hot spots corresponding to visible tumours (Fig. 4c, d). Furthermore, targeting was prevented by
a 30-fold excess of unlabelled AnnA1 IgG but not by control IgG (data not shown). Region-of-interest and
biodistribution analysis confirmed targeting in vivo with an average tumour accumulation at two hours of 34%
injected dose per gram of tissue. This compared favourably to VEGF receptor antibodies which accumulated at
6.4% injected dose per gram of tumour. When injected into rats without tumours, 125I-AnnA1 antibodies showed no
targeting of normal organs, including lung at levels less than 1% injected dose per gram of tissue, whereas
VEGF receptor antibody accumulation was greater in multiple organs (data not shown). The uptake ratio in rat
tumour-bearing lungs versus normal lungs was up to 2.0 and 70 for antibodies to VEGF receptor and AnnA1,
respectively. Thus, -scintigraphic imaging rapidly validated AnnA1 as a tumour target that is readily
accessible to antibody injected intravenously for tumour targeting and imaging in vivo. AnnA1 appeared to be
selectively externalized on the endothelial cell surface in the solid tumours.
Figure 4 Tumour-specific targeting of 125I-AnnA1 antibodies after intravenous injection into tumour-bearing
rats. Full legend
High resolution image and legend (23k)
Radio-immunotherapy of solid tumours
Many tumour-bearing rats imaged with the 125I-AnnA1 antibody survived, so we performed a survival study and
recorded animal body weights; 80% of the animals treated with the 125I-AnnA1 antibody survived 8 days or longer
compared with the 125I-IgG-treated and untreated rats, which died within 7 days (Fig. 5a). The body weights of
all tumour-bearing rats began to drop 7–10 days after tumour cell inoculation (Fig. 5b). The control rats
continued to decrease in body weight to 23–30% less than normal at their death. In contrast, rats treated with
125I-AnnA1 IgG began to gain weight within 3–4 days and reached a normal body weight after 25 days. This
increased survival was striking because in this model many animals die within 2–4 days of treatment and thus
may lack sufficient time to benefit from treatment. The survival rate of rats surviving the first week
approached 90%. The one rat that died after 2 weeks required euthanasia because of a leg tumour and large tail
tumour that were not apparent when treated. Thus, a single injection of 125I-AnnA1 antibody caused significant
remission even in advanced disease.
Figure 5 AnnA1 targeted radio-immunotherapy increases survival in rats. Full legend
High resolution image and legend (22k)
AnnA1 in human tumour neovasculature
We immuno-stained tissue sections of human solid tumours. AnnA1 antibody labelled blood vessels of human
prostate, liver, breast and lung tumours but not matched normal tissues (Fig. 6). Antibodies to platelet
endothelial cell adhesion molecule-1 (PECAM) stained both normal and tumour blood vessels. The lack of AnnA1
expression in vascular endothelium of multiple normal organs has been reported previously42-45. Thus, AnnA1 was
selectively detected on the neovascular endothelium of multiple human solid tumours.
Figure 6 Expression of AnnA1 on vascular endothelium of multiple primary human solid tumours. Full legend
High resolution image and legend (99k)
Discussion
We describe a new logic-based discovery and validation approach that integrates newly developed, global
analytical techniques to map the proteins expressed in vivo at the luminal endothelial cell surface. This
approach has demonstrated distinct molecular signatures in normal and neoplastic tissues. We applied this
strategy to rat lungs and solid tumours to uncover, from the vast number of proteins expressed in tissue,
approximately 50 differentially expressed proteins, including two promising tissue-selective endothelial cell
surface proteins that permitted rapid and specific immuno-targeting and imaging in vivo. Profiling the
endothelial cell surface that is accessible in vivo is an important logical step for validating the hypothesis
of tissue-modulated endothelial cell diversity in vivo and for discovering potential targets. This is important
not only to direct pharmacodelivery and molecular imaging but also—by means of caveolae—to overcome the
restrictive endothelial cell barrier to transport drugs or genes to the underlying tissue cells16, 17.
Key features of our analysis included tissue subfractionation with subtractive proteomic and bioinformatic
filters that together reduced tissue complexity by greater than five orders of magnitude, and unmasked a
manageable subset of proteins at the inherently accessible blood–tissue interface. This has led to the
creation of a database of vascular endothelial cell surface proteins containing accessible proteins apparently
modulated by the tissue. After bioinformatic filtering, western blot analysis and/or tissue immuno-staining
provided sensitive expression profiling to yield only a few candidate proteins exhibiting organ- or
tumour-specificity. Planar and SPECT imaging, using intravenously injected antibodies specific to each protein,
visualized targeting and tissue accumulation with high sensitivity and resolution. Imaging thus provided a
rigorous and objective validation of accessibility and tissue-specificity of the few remaining candidate
targets and ultimately demonstrated potential utility such as, how rapidly and to what extent the antibody
targets single organs or solid tumours in vivo.
So far, in vivo imaging correlates well with the expression profiling using isolated endothelial plasma
membranes. It showed lung-specific immuno-targeting for APP (Fig. 2), tumour-specificity for AnnA1 (Fig. 4) and
targeting of multiple tissues for less specific target proteins (that is, PV-1, VEGF-R and podocalyxin) (our
unpublished observations). Because of poor access inside many tissues, antibodies injected intravenously
usually require significantly higher doses (250 µg kg-1 (ref. 46) compared with 20 µg kg-1 used here) to get a
small percentage into the tissue that binds and can then be visualized clearly a day or so later, after the
background signal has been cleared from the blood. Here, the binding was direct and unhindered by barriers so
that both tissue accumulation and blood clearance were rapid, thereby providing striking images within minutes
to hours. The rapidity and high levels of specific targeting observed here meet the theoretical expectation of
the vascular targeting strategy17. Although fast emerging as a standard for assessing targeting and
specificity1-4, whole-body imaging may be underutilized in target validation despite being non-invasive and
highly sensitive.
Using a new, integrated analytical approach we have found new tissue-specific endothelial cell surface proteins
that can act as vascular targets to bring us one step closer to achieving the century-old elusive goal of
targeting single organs or solid tumours in vivo1, 2, 4, 6, 10. The development and optimization of several key
technologies has provided the sensitivity and throughput required for this new target discovery and validation
process. We expect that site-directed vascular and caveolar targeting will benefit both drug and gene delivery
in the treatment of many diseases16. We have demonstrated here, using a rat tumour model that monoclonal
antibodies to AnnA1 can effectively direct low levels of radionuclides (100 µCi) to concentrate in, and thus
destroy solid tumours, which ultimately increases animal survival. Because AnnA1 is also selectively detected
in multiple human solid tumours, this target may similarly help to image and treat human disease.
Methods
A detailed description of the materials, 2D gel analysis, expression profiling in vivo of candidate proteins,
rat tumour models, -scintigraphic imaging and biodistribution analysis is available in Supplementary Methods.
Proteomic analysis We used a three-pronged approach to resolve proteins/peptides for mass spectrometric
analysis: (1) The proteins of silica-coated luminal endothelial cell plasma membranes and caveolae isolated
from various normal organs or tumours were resolved by high resolution 2D gel analysis before excising
potential organ- or tumour-specific protein spots for mass spectrometric analysis; (2) Proteins in the isolated
endothelial plasma membranes and caveolae were separated using one-dimensional (1D) SDS–polyacrylamide gel
electrophoresis (SDS–PAGE) and specific bands of interest were cut out or the whole gel lane was cut into 50
slices, and the proteins in each of the gel slices were analysed by mass spectrometry; and (3)
Multi-dimensional Protein Identification Technology (MudPIT) was used to analyse tryptic peptides from a
complex mixture of proteins extracted directly from the whole isolated endothelial plasma membrane fraction and
caveolae isolates. Each gel spot/slice was de-stained and digested overnight with trypsin before extracting the
cleaved peptides from the gel and then loading them onto a reverse phase micro-column for gradient acetonitrile
elution directly into the mass spectrometer (LCQ Deca XP ion trap mass spectrometer (ThermoFinnigan) equipped
with a modified micro-electrospray ionization source from Mass Evolution). For MudPIT, 150 µg of complex
peptide mixture was separated by 2D liquid chromatography, comprising a micro-column packed with three phases
of chromatographic material as follows: 8.5 cm of 5 µm reversed phase material (Polaris C18-A, Metachem); 4 cm
of 5 µm 300 Å strong cation exchanger (PolyLC); and lastly 3.5 cm of C18 material, using a helium pressure cell
operated at 600–900 psi (Mass Evolution). Peptides were directly eluted into the mass spectrometer using 2D
chromatography with 18 step-elutions from the strong cation exchanger, followed by a gradient elution of the
reversed phase material. Operation of the quarternary Agilent 1100 HPLC pump and the mass spectrometer was
fully automated during the entire procedure using the Excalibur 1.2 data system (ThermoFinnigan). Continuous
cycles of one full scan (m/z 400 to 1,400) followed by three data-dependent MS/MS measurements at 35%
normalized collision energy were performed. MS/MS measurements were allowed for the three most intense
precursor ions with an enabled exclusion list of 25 m/z values ( 1.5 Da) or a maximum time limit of 5 min. The
zoom scan function to determine the charge state was disabled in order to increase the duty cycle of the
instrument.
Database search and in silico analysis of tandem mass spectra MS/MS spectra were extracted from raw files
requiring a minimum of 21 signals with an intensity of at least 4.75 104 arbitrary units (AU). Extracted MS/MS
spectra were automatically assigned to the best matching peptide sequence using the SEQUEST algorithm and the
Sequest Browser software package (ThermoFinnigan). SEQUEST searches were performed using a rat protein database
containing 40,800 protein sequences that were downloaded as FASTA formatted sequences from ENTREZ (National
Center for Biotechnology Information (NCBI); http://www.ncbi.nlm.nih.gov/Entrez). Sequence redundancies were
removed using Perl script. The peptide mass search tolerance was set to 3 Da. Spectral matches were retained
with a minimal cross-correlation score (XCorr) of 1.5, 2.2 and 3.3 for charge states +1, +2 and +3,
respectively. DeltaCN (top match's XCorr minus the second-best match's XCorr, divided by top match's XCorr) had
to be equal or less than 0.07. Retained spectral matches were filtered and re-assigned to proteins using
DTASelect. DTASelect outputs of independent measurements were entered into the AVATAR database. AVATAR was
designed to store a large amount of mass spectrometric data and to provide tools to analyse the data to extract
valuable information. We used relational models for database design based on entity relationship and
implemented the database in the MySQL relational database management system (MySQL) to support database query
and management. This relational database plus the Perl-based interface greatly improved data organization, data
consistency and integrity, and facilitated data comparison and information retrieval. In the case of the 1D gel
and MudPIT approaches, AVATAR was used to subtract the data to find proteins detected only at the lung
endothelial cell surface in vivo versus in vitro or on the tumour but not normal endothelium.
In silico bioinformatic interrogation To identify possible candidates for intravenously accessible targets from
the subset of proteins identified as lung or tumour induced, we determined their currently known
membrane-associated structure (bilayer spanning versus lipid anchor (intra- or extracellular) versus peripheral
interaction) from scientific reports and/or protein databases, such as SwissProt
(http://us.expasy.org/sprot/sprot-top.html) and the NCBI ENTREZ protein database
(http://www.ncbi.nlm.nih.gov/entrez/query.fcgi). We also used web-based prediction programs to identify
candidates that may harbour transmembrane spanning alpha helices (Prediction of Transmembrane Regions and
Orientation (TMpred), http://www.ch.embnet.org/software/TMPRED_form.html) or glycosylation sites to indicate a
possible ectodomain exposed to the circulating blood (Prosite Scan,
http://npsa-pbil.ibcp.fr/cgi-bin/npsa_automat.pl?page = npsa_prosite.html). Only 100% probabilities were taken
into consideration.
Supplementary information accompanies this paper.
Received 28 January 2004;accepted 19 April 2004
References 1. Massoud, T. F. & Gambhir, S. S. Molecular imaging in living subjects: seeing fundamental
biological processes in a new light. Genes Dev. 17, 545–580 (2003) | Article | PubMed | ISI | ChemPort |
2. Herschman, H. R. Molecular imaging: looking at problems, seeing solutions. Science 302, 605–608 (2003) |
Article | PubMed | ISI | ChemPort |
3. Rudin, M. & Weissleder, R. Molecular imaging in drug discovery and development. Nature Rev. Drug Discov. 2,
123–131 (2003) | Article | PubMed | ISI | ChemPort |
4. Weissleder, R. Scaling down imaging: molecular mapping of cancer in mice. Nature Rev. Cancer 2, 11–18
(2002) | Article | PubMed | ISI | ChemPort |
5. Drews, J. Drug discovery: a historical perspective. Science 287, 1960–1964 (2000) | Article | PubMed | ISI
| ChemPort |
6. Lindsay, M. A. Target discovery. Nature Rev. Drug Discov. 2, 831–838 (2003) | Article | PubMed | ISI |
ChemPort |
7. Workman, P. New drug targets for genomic cancer therapy: successes, limitations, opportunities and future
challenges. Curr. Cancer Drug Targets 1, 33–47 (2001) | PubMed | ChemPort |
8. Anzick, S. L. & Trent, J. M. Role of genomics in identifying new targets for cancer therapy. Oncology
(Huntingt.) 16, 7–13 (2002) | PubMed |
9. Cavenee, W. K. Genetics and new approaches to cancer therapy. Carcinogenesis 23, 683–686 (2002) | Article |
PubMed | ISI | ChemPort |
10. Huber, L. A. Is proteomics heading in the wrong direction? Nature Rev. Mol. Cell Biol. 4, 74–80 (2003) |
Article | PubMed | ISI | ChemPort |
11. Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752 (2000) | Article |
PubMed | ISI | ChemPort |
12. Jain, R. K. The next frontier of molecular medicine: delivery of therapeutics. Nature Med. 4, 655–657
(1998) | Article | PubMed | ISI | ChemPort |
13. Dvorak, H. F., Nagy, J. A. & Dvorak, A. M. Structure of solid tumors and their vasculature: implications
for therapy with monoclonal antibodies. Cancer Cells 3, 77–85 (1991) | PubMed | ISI | ChemPort |
14. von Mehren, M., Adams, G. P. & Weiner, L. M. Monoclonal antibody therapy for cancer. Annu. Rev. Med. 54,
343–369 (2003) | Article | PubMed | ISI | ChemPort |
15. Farah, R. A., Clinchy, B., Herrera, L. & Vitetta, E. S. The development of monoclonal antibodies for the
therapy of cancer. Crit. Rev. Eukaryot. Gene Expr. 8, 321–356 (1998) | PubMed | ISI | ChemPort |
16. Carver, L. A. & Schnitzer, J. E. Caveolae: mining little caves for new cancer targets. Nature Rev. Cancer
3, 571–581 (2003) | Article | PubMed | ISI | ChemPort |
17. Schnitzer, J. E. Vascular targeting as a strategy for cancer therapy. N. Engl. J. Med. 339, 472–474 (1998)
| Article | PubMed | ISI | ChemPort |
18. Madri, J. A. & Williams, S. K. Capillary endothelial cell culture: Phenotype modulation by matrix
components. J. Cell Biol. 97, 153–165 (1983) | Article | PubMed | ISI | ChemPort |
19. Schnitzer, J. E. in Vascular Endothelium: Physiology, Pathology and Therapeutic Opportunities (eds Born, G.
V. R. & Schwartz, C. J.) 77–95 (Schattauer, Stuttgart, 1997)
20. Aird, W. C. et al. Vascular bed-specific expression of an endothelial cell gene is programmed by the tissue
microenvironment. J. Cell Biol. 138, 1117–1124 (1997) | Article | PubMed | ISI | ChemPort |
21. Janzer, R. C. & Raff, M. C. Astrocytes induce blood–brain barrier properties in endothelial cells. Nature
325, 253–257 (1987) | Article | PubMed | ISI | ChemPort |
22. Stewart, P. A. & Wiley, M. J. Developing nervous tissue induces formation of blood-brain barrier
characteristics in invading endothelial cells: a study using quail-chick transplantation chimeras. Dev. Biol.
84, 183–192 (1981) | PubMed | ISI | ChemPort |
23. Auerbach, R. et al. Specificity of adhesion between murine tumor cells and capillary endothelium: an in
vitro correlate of preferential metastasis in vivo. Cancer Res. 47, 1492–1496 (1987) | PubMed | ISI | ChemPort
|
24. Pasqualini, R. & Ruoslahti, E. Organ targeting in vivo using phage display peptide libraries. Nature 380,
364–366 (1996) | Article | PubMed | ISI | ChemPort |
25. Rajotte, D. et al. Molecular heterogeneity of the vascular endothelium revealed by in vivo phage display.
J. Clin. Invest. 102, 430–437 (1998) | PubMed | ISI | ChemPort |
26. Papetti, M. & Herman, I. M. Mechanisms of normal and tumor-derived angiogenesis. Am. J. Physiol. Cell
Physiol. 282, C947–C970 (2002) | PubMed | ISI | ChemPort |
27. Ferrara, N. VEGF and the quest for tumour angiogenesis factors. Nature Rev. Cancer 2, 795–803 (2002) |
Article | PubMed | ISI | ChemPort |
28. Kerbel, R. & Folkman, J. Clinical translation of angiogenesis inhibitors. Nature Rev. Cancer 2, 727–739
(2002) | Article | PubMed | ISI | ChemPort |
29. St Croix, B. et al. Genes expressed in human tumor endothelium. Science 289, 1197–1202 (2000) | Article |
PubMed | ISI | ChemPort |
30. Huang, X. et al. Tumor infarction in mice by antibody-directed targeting of tissue factor to tumor
vasculature. Science 275, 547–550 (1997) | Article | PubMed | ISI | ChemPort |
31. McIntosh, D. P., Tan, X.-Y., Oh, P. & Schnitzer, J. E. Targeting endothelium and its dynamic caveolae for
tissue-specific transcytosis in vivo: A pathway to overcome cell barriers to drug and gene delivery. Proc. Natl
Acad. Sci. USA 99, 1996–2001 (2002) | Article | PubMed | ChemPort |
32. Sipkins, D. A. et al. Detection of tumor angiogenesis in vivo by alphaVbeta3-targeted magnetic resonance
imaging. Nature Med. 4, 623–626 (1998) | Article | PubMed | ISI | ChemPort |
33. Hu, Z. & Garen, A. Targeting tissue factor on tumor vascular endothelial cells and tumor cells for
immunotherapy in mouse models of prostatic cancer. Proc. Natl Acad. Sci. USA 98, 12180–12185 (2001) | Article
| PubMed | ChemPort |
34. Hood, J. D. et al. Tumor regression by targeted gene delivery to the neovasculature. Science 296, 2404–
2407 (2002) | Article | PubMed | ISI | ChemPort |
35. Oh, P. & Schnitzer, J. E. in Cell Biology: A Laboratory Handbook (ed. Celis, J.) 34–36 (Academic Press,
Orlando, 1998)
36. Schnitzer, J. E., McIntosh, D. P., Dvorak, A. M., Liu, J. & Oh, P. Separation of caveolae from associated
microdomains of GPI-anchored proteins. Science 269, 1435–1439 (1995) | PubMed | ISI | ChemPort |
37. Schnitzer, J. E. gp60 is an albumin-binding glycoprotein expressed by continuous endothelium involved in
albumin transcytosis. Am. J. Physiol. 262, H246–H254 (1992) | PubMed | ISI | ChemPort |
38. Henniker, A. J., Bradstock, K. F., Grimsley, P. & Atkinson, M. K. A novel non-lineage antigen on human
leucocytes: characterization with two CD-48 monoclonal antibodies. Dis. Markers 8, 179–190 (1990) | PubMed |
ISI | ChemPort |
39. Essler, M. & Ruoslahti, E. Molecular specialization of breast vasculature: a breast-homing phage-displayed
peptide binds to aminopeptidase P in breast vasculature. Proc. Natl Acad. Sci. USA 99, 2252–2257 (2002) |
Article | PubMed | ChemPort |
40. Perillo, N. L., Marcus, M. E. & Baum, L. G. Galectins: versatile modulators of cell adhesion, cell
proliferation, and cell death. J. Mol. Med. 76, 402–412 (1998) | Article | PubMed | ISI | ChemPort |
41. Gerke, V. & Moss, S. E. Annexins: from structure to function. Physiol. Rev. 82, 331–371 (2002) | PubMed |
ISI | ChemPort |
42. Dreier, R., Schmid, K. W., Gerke, V. & Riehemann, K. Differential expression of annexins I, II and IV in
human tissues: an immunohistochemical study. Histochem. Cell Biol. 110, 137–148 (1998) | Article | PubMed |
ISI | ChemPort |
43. Eberhard, D. A., Brown, M. D. & VandenBerg, S. R. Alterations of annexin expression in pathological
neuronal and glial reactions. Immunohistochemical localization of annexins I, II (p36 and p11 subunits), IV,
and VI in the human hippocampus. Am. J. Pathol. 145, 640–649 (1994) | PubMed | ISI | ChemPort |
44. Ahn, S. H., Sawada, H., Ro, J. Y. & Nicolson, G. L. Differential expression of annexin I in human mammary
ductal epithelial cells in normal and benign and malignant breast tissues. Clin. Exp. Metastasis 15, 151–156
(1997) | Article | PubMed | ISI | ChemPort |
45. McKanna, J. A. & Zhang, M. Z. Immunohistochemical localization of lipocortin 1 in rat brain is sensitive to
pH, freezing, and dehydration. J. Histochem. Cytochem. 45, 527–538 (1997) | PubMed | ISI | ChemPort |
46. Bredow, S., Lewin, M., Hofmann, B., Marecos, E. & Weissleder, R. Imaging of tumour neovasculature by
targeting the TGF-beta binding receptor endoglin. Eur. J. Cancer 36, 675–681 (2000) | Article | PubMed | ISI |
ChemPort |
Acknowledgements. We thank A. Wempren, K. Hearn, M. Bourne, L. Randall and T. Smith for technical assistance.
This research was supported by the National Institute of Health (Heart, Lung and Blood), National Cancer
Institute, Sidney Kimmel, Schutz Foundation, California Tobacco-related Disease Research Program and California
Breast Cancer Research Program.
Competing interests statement. The authors declare that they have no competing financial interests
按:蛋白质组学的技术可以是我们鉴定大量的差异蛋白,但是这也给进一步确证工作带来了巨大的压力。蛋白质组学不仅要做
到多,还应该进一步做到少。这种由少到多再到少,是一个升华。