相关产品推荐更多 >
万千商家帮你免费找货
0 人在求购买到急需产品
- 详细信息
- 询价记录
- 文献和实验
- 技术资料
- 保存条件:
负20℃
- 英文名:
Sheep Anti-Rat Isolated Glomerular Basement Membrane (Anti-GBM) Serum
- 库存:
1
- 供应商:
北京博蕾德生物科技有限公司
- 规格:
25ml
绵羊抗大鼠肾小球基底膜血清(PTX-001AGBM)
Sheep Anti Rat Glomerular Basement Membrane (GBM) Serum
--抗GBM型肾炎模型诱导
| 产品名称 | Sheep Anti Rat Glomerular Basement Membrane (GBM) Serum |
| 货号 | PTX-001AGBM |
| 规格 | 25ml |
| 保存 | -20℃ |
| 说明 | 产品经56℃热处理30min,请避免反复冻融。解冻后会有轻微沉淀,注射前3000-5000rmp 离心30min。 注:只做过大鼠炎症,没有做过小鼠验证。 |
每瓶血清含有足够的抗体用于诱导至少25只大鼠*(175-200 g体重)被动抗GBM肾炎模型。应用说明:(实验前请仔细阅读实验流程)
免疫抗GMB血清:麻醉大鼠,尾静脉注射抗GMB血清超过15秒,疾病的产生依赖于免疫剂量,依照免疫剂量完全打入体内很关键(推荐用量:0.4-0.5ml/100g体重)。由于不同批次抗血清差异,大鼠来源,以及实验要求的不同,我们建议进行剂量-反应研究,具体的免疫剂量和疾病的严重程度,需要根据每个不同批次血清和产生疾病的严重程度,选择合适的免疫剂量。
肾病研究:
1)异源性疾病:免疫抗GBM (anti GBM)3-5天后,免疫荧光检测显示绵羊IgG在肾小球基底膜内呈线状沉积。大鼠c3也呈线性分布,24小时后出现蛋白尿。
2)自身疾病:免疫抗GBM抗体8-10天后,检测大鼠蛋白尿增加,同时大鼠肾小球IgG(自身抗体) 呈线状沉积,自体疾病变得明显。(自体)免疫组化呈线性模式的IgG(图1)。到3周时,蛋白尿有望达到200毫克/24小时,肾小球病变(图2)明显,随着时间的推移,严重程度增加,导致肾小球硬化。
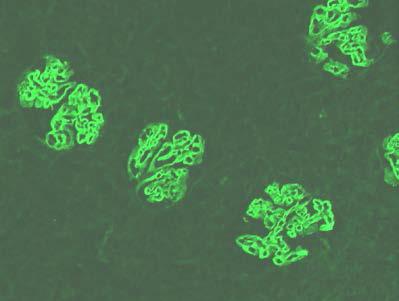
图1.免疫荧光检测显示免疫抗GBM3周后肾小球毛细血管壁大鼠IgG免疫沉积的。
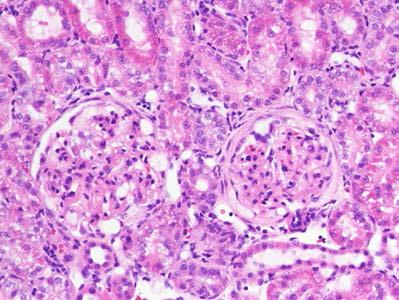
图2.免疫组化染色显示免疫抗GBM 3周后新月体形成、系膜细胞增生、毛细血管变形。
相关产品:
| 货号 |
产品名称 |
规格 |
| 肾炎模型 |
||
| PTX-001AGBM |
Sheep Anti-Rat GBM Serum |
25ml |
| PTX-002S |
Sheep Anti-Rat Fx1A Serum |
25ml |
| PTX-003S |
Sheep Anti-Rat Thy-1 Serum |
20ml |
| PTX-000S |
Sheep Non-Immune Serum |
25ml |
| 组织产品(动物疾病模型组织、切片、血浆、尿液) |
||
| PTX-001 |
Anti-GBM (Immune-mediated Glomerulonephritis) |
- |
| PTX-002 |
Anti-Fx1A (Heymann Nephritis, Membranous Nephritis) |
- |
| PTX-003. |
Anti-Thy-1 (Mesangial Proliferative Glomerulonephritis) |
- |
| PTX-004 |
Diabetic nephropathy (streptozotocin- Type I Diabetes) |
- |
| PTX-005 |
Control (Normal) Kidney |
- |
| PTX-006 |
Sheep Kidney Section(anti-GBM and Fx1A membranous nephropathy |
- |
| 细胞 |
||
| CRGMes-1 |
Rat Glomerular Mesangial Cells |
1x106 |
| CRGEp-1 |
Rat Glomerular Epithelial Cells |
1x106 |
| CBGEn-1 |
Bovine Glomerular Endothelial Cells |
1x106 |
| CMUB-1 |
Mouse Ureteric Bud Cells |
1x106 |
| CMMM-1 |
Mouse Metanephric Mesynchymal Cells |
1x106 |
| CRMM-1 |
Rat Metanephric Mesynchymal Cells |
1x106 |
| 抗体 |
||
| BS-001GBM |
FITC- Sheep Anti-Glomerular Basement Membrane IgG |
0.5ml |
| BS-002ECM |
FITC- Sheep Anti-Extracellular Matrix (ECM) IgG |
0.5ml |
参考文献:
1.McIntosh LM, Barnes JL, Barnes VL, McDonald JR. Selective CCR2-targeted macrophage depletion ameliorates experimental mesangioproliferative glomerulonephritis. Clin Exp Immunol 155:295-303, 2009. Osprey Pharma, Probetex, Inc. (Contract Research, Pre-Clinical Testing, Histopathology)
2.Velagapudi C, Nilsson R-P, Barnes VL, Arar M, Abboud HE, Barnes JL. Reciprocal induction of simple organogenesis by mouse kidney progenitor cells in three-dimensional co-culture. Am J Pathol 180:819-830, 2012. Link (Cover Photo, February Issue). Probetex, Inc, Univ TX Hlth Sci Ctr, San Antonio, TX. (CMMM-1 and CMUB-1: Mouse Kidney Primordial Cells).
3.Riser BL, Najmabadi F, Garchow K, Barnes JL, Peterson DR, Sukowski EJ: Treatment with matricellular protein CCN3 blocks and/or reverses fibrosis development in obesity with diabetic nephropathy. Am J Pathol 184:2908–2921, 2014. Rosalind Franklin University of Medicine and Science, Baxter Healthcare, Probetex, Inc. (Histopathology, Image Analysis).
4.Sun H, Olsen HS, Merigeon EY, So E, Burch E, Kinsey S, Papadimitriou JC, Drachenberg CB, Bentzen SM, Block DS, Strome SE, Zhang X: Recombinant human IgG1 based Fc multimers, with limited FcR bindng capacity, can effectively inhibit complement-mediated disease. J Autoimmun 84: 87-98, 2017. (rats) University of Maryland School of Medicine, Gliknik, Inc., Chengdu Military General Hospital China.
5.Patel M, Velagapudi C, Burns HS, Doss R, Lee, MJ, Mariappan M, Wagner B, Arar M, Barnes VL, Abboud HE, Barnes JL. Mouse metanephric mesenchymal cell-derived angioblasts undergo vasculogenesis in three-dimensional culture. Am J Pathol 188: 768-784, 2018. Probetex, Inc, Univ TX Hlth Sci Ctr, San Antonio, TX. (CMMM-1 and CMUB-1: Mouse Kidney Primordial Cells).
6.Rufanova VA, Lianos E, Alexanian A, Sorokina E, Sharma M, McGinty A, Sorokin A: G3G overexpression in glomerular epithelial cells during anti-GBM-induced glomerulonephritis. Kidney Int 75:31-40, 2009. (mice) (Medical College of Wisconsin).
7.Lichtnekert J, Kulkarni OP, Mulay SR, Rupanagudi KV, Ryu M, Allam R, Vielhauer V, Muruve D, Lindenmeyer MT, Cohen CD, Anders H-J. Anti-GBM glomerulonephritis involves IL-1 but is independent of NLRP3/ASC inflammasome-mediated activation of caspase-1. PLoS ONE 6(10): e26778. doi:10.1371/journal.pone.0026778. October 2011. (mice) (Ludwig-Maximillians-Univeristy of Munich).
8.Schwarz M, Taubitz A, Eltrich N, Mulay SR, Allam R, Vielhauer V: Analysis of TNF-mediated recruitment and activation of glomerular dendritic cells in mouse kidneys by compartment-specific flow cytometry. Kidney Int 84: 116-129, 2013. (mice) (Ludwig-Maximillians-Univeristy of Munich).
9.Kim J, Imig JD, Yang J, Hammock BD, Padanilam BJ: Inhibition of soluble epoxide hydrolase prevents renal interstitial fibrosis and inflammation. Am J Physiol Renal Physiol 307: F971-F980, 2014. (mice). (University of Nebraska USA).
10.Zheng W, Warner R, Ruggeri R, Su C, Cortes C, Skoura A, Ward J, Ahn K, Kalgutkar A, Sun D, Maurer TS, Bonin PD, Okerberg C, Bobrowski W, Kawabe T, Zhang Y, Coskran T, Bell S, Kapoor B, Johnson K, Buckbinder L. PF-1355, a mechanism-based myeloperoxidase inhibitor, prevents immune complex vasculitis and anti–glomerular basement membrane glomerulonephritis. J Pharmacol Exp Ther 353:288–298, 2015. (mice). Pfizer and University of Michigan.
11.Pavkovic M, Riefke B, Frisk AL, Gröticke I, Ellinger-Ziegelbauer H. Glomerulonephritis-induced changes in urinary and kidney MicroRNA profiles in rats. Toxicol Sci. 145(2), 348–359, 2015. (Rats). Bayer Pharma AG and Harvard Medical School.
12.Kumar SV, Kulkarni OP, Mulay SR, Darisipudi MN, Romoli S, Thomasova D, Scherbaum CR, Hohenstein B, Hugo C, Müller S, Liapis H, Anders HJ. Neutrophil Extracellular Trap-Related Extracellular Histones Cause Vascular Necrosis in Severe GN. J Am Soc Nephrol. 26 (10):2399-2413, 2015 (mice) (Ludwig-Maximilians-University of Munich, Munich).
13.Bosma M, Gerling M, Pasto J, Georgiadi A, Graham E, Shilkova O, Iwata Y, Almer S, Soderman J, Toftgard R, Wermeling F, Bostrom EA, Bostrom PA. FNDC4 acts as an anti-inflammatory factor on macrophages and improves colitis in mice. Nature Commun 7: 11314. Apr 12 2016. (mice) Karolinska Institute, Stockholm Sweden
14.Mulay SR, Romoli S, Desai J, Honarpischeh, MM, Kumar SV, Anders H-J. Murine double minute-2 inhibition ameliorates established crescentic glomerulonephritis. Am J Pathol. 186: 1442-153, 2016. (mice) Medizinische Klinik und Poliklinik University Hoispital of Ludwig-Maximillians-University , Munich, Germany.
15.Hachmo Y, Kalechman Y, Skornick I, Gafter U, Caspi RR, and Sredni B: The small tellurium compound AS101 ameliorates rat crescentic glomerulonephritis: association with inhibition of macrophage caspase-1 activity via very late antigen-4 inactivation. Front Immunol. 8: 240-, 2017. doi: 10.3389/immu.2017.00240 PMCID: PMC5339302. (Rats) C.A.I.R. Institute, The Safdiè AIDS and Immunology Research Center; Laboratory of Immunology, National Eye Institute, National
Institutes of Health, Bethesda, MD, USA
16.Hsu M-F, Betaieb A, Ito Y, Graham J, Havel PJ, Haj FG. Protein tyrosine phosphatase Shp2 deficiency in podocytes attenuates lipopolysaccharide-induced proteinuria. Scientific Reports 7: 461 2017. (mice). UC-Davis Univ Tennessee-Knoxville Tennessee, USA.
17.Velez JCQ, Arif E, Rodgers J, Hicks MP, Arthur JM, Nihalani D, Bruner ET, Budisavljevic MN, Atkinson C, Fitzgibbon WR, Janech MG. Deficiency of the angiotensinase aminopeptidase A increases susceptibility to glomerular injury. J Am Soc Nephrol: 28(7):2119-2132, 2017. (mice). Ochsner Clinic Foundation, New Orleans, LA, Medical University of South Carolina, Charleston, SC, Augusta University, Augusta, GA, University of Arkansas for Medical Sciences, Little
Rock, AR
18.Bettaieb A, Koike S, Chahed S, Zhao Y, Bachaalany S, Hashoush N, Graham J, Fatima H, Havel PJ, Gruzdev A, Zeldin DC, Hammock BD, Haj FG. Podocyte-specific soluble epoxide hydrolase deficiency in mice attenuates acute kidney injury. FEBS J. 284(13):1970-1986, 2017.(mice). UC Davis, Univ of Tenn-Knoxville, NIEHS PMCID:
19.Wen Y, Lu X, Ren J, Privratsky JR, Yang B, Rudemiller NP, Zhang J, Griffiths R, Jain MK, Nedospasov SA, Liu BC, Crowley SD. KLF4 in macrophages attenuates TNFα-mediated kidney injury and fibrosis. J Am Soc Nephrol. 30:1925-1938, 2019. (mice). Duke University Medical Center, Duke-National University of Singapore, Durham Veterans Affairs Medical Center.
风险提示:丁香通仅作为第三方平台,为商家信息发布提供平台空间。用户咨询产品时请注意保护个人信息及财产安全,合理判断,谨慎选购商品,商家和用户对交易行为负责。对于医疗器械类产品,请先查证核实企业经营资质和医疗器械产品注册证情况。
- 作者
- 内容
- 询问日期
 文献和实验
文献和实验PTX-001: Sheep Anti-Glomerular Basement Membrane (GBM) Serum:
Alli AA, Desai D, Elshika A, Conrad M, Proneth B, Clapp W, Atkinson C, Segal M, Searcy LA, Denslow ND, Bolisetty S, Mehrad B, Morel L, Scindia Y. Kidney tubular epithelial cell ferroptosis links glomerular injury to tubulointerstitial pathology in lupus nephritis. Clin Immunol. Volume 248, March 2023, in press. Epub ahead of print. PMID: 36566913. (Mice)
Fayçal CA, Oszwald A, Feilen T, Cosenza-Contreras M, Schilling O, Loustau T, Steinbach F, Schachner H, Langer B, Heeringa P, Rees AJ, Orend G, Kain R. An adapted passive model of anti-MPO dependent crescentic glomerulonephritis reveals matrix dysregulation and is amenable to modulation by CXCR4 inhibition. Matrix Biol. 106:12-33, 2022. Epub 2022 Jan 13. PMID: 35032611. (Mice)
Kim K, Na M, Oh K, Cho E, Han SS, Chang S. Optimized single-step optical clearing solution for 3D volume imaging of biological structures. Commun Biol. 5:431-441, 2022. PMID: 35534680; PMCID: PMC9085829. (Mice)
Butt L, Unnersjö-Jess D, Höhne M, Hahnfeldt R, Reilly D, Rinschen MM, Plagmann I, Diefenhardt P, Brähler S, Brinkkötter PT, Brismar H, Blom H, Schermer B, Benzing T. Super-resolution imaging of the filtration barrier suggests a role for podocin r229q in genetic predisposition to glomerular disease. J Am Soc Nephrol. 33:138-154, 2022. PMID: 34853150. (Mice)
Melica ME, Antonelli G, Semeraro R, Angelotti ML, Lugli G, Landini S, Ravaglia F, Regina G, Conte C, De Chiara L, Peired AJ, Mazzinghi B, Donati M, Molli A, Steiger S, Magi A, Bartalucci N, Raglianti V, Guzzi F, Maggi L, Annunziato F, Burger A, Lazzeri E, Anders HJ, Lasagni L, Romagnani P. Differentiation of crescent-forming kidney progenitor cells into podocytes attenuates severe glomerulonephritis in mice. Sci Transl Med. 14657: 2022. PMID: 35947676; PMCID: PMC7614034. (Mice).
Rousselle A, Sonnemann J, Amann K, Mildner A, Lodka D, Kling L, Bieringer M, Schneider U, Leutz A, Enghard P, Kettritz R, Schreiber A. CSF2-dependent monocyte education in the pathogenesis of ANCA-induced glomerulonephritis. Ann Rheum Dis. 81:1162-1172, 2022. PMID: 35418479; PMCID: PMC9279749. (Mice)
Bjørnholm KD, Ougaard ME, Skovsted GF, Knudsen LB, Pyke C. Activation of the renal GLP-1R leads to expression of Ren1 in the renal vascular tree. Endocrinol Diabetes Metab. 19;4:e00234, 2021. PMID: 34277961; PMCID: PMC8279630. (Mice)
Pagan JD, Vlamakis H, Gaca A, Xavier RJ, Anthony RM. Modulating T follicular cells in vivo enhances antigen-specific humoral immunity. J Immunol. 206:2583-2595, 2021. PMID: 34011521; PMCID: PMC8164984. (Mice)
Ren J, Xu Y, Lu X, Wang L, Ide S, Hall G, Souma T, Privratsky JR, Spurney RF, Crowley SD. Twist1 in podocytes ameliorates podocyte injury and proteinuria by limiting CCL2-dependent macrophage infiltration. JCI Insight. 6:e148109, 2021. PMID: 34369383; PMCID: PMC8410065. (Mice)
Möller-Hackbarth K, Dabaghie D, Charrin E, Zambrano S, Genové G, Li X, Wernerson A, Lal M, Patrakka J. Retinoic acid receptor responder1 promotes development of glomerular diseases via the Nuclear Factor-κB signaling pathway. Kidney Int. 100:809-823, 2021. PMID: 34147551. (Mice).
Commentary to Moller: Chen A, Lee K, He JC. Autocrine and paracrine effects of a novel podocyte gene, RARRES1. Kidney Int. 100:745-747, 2021. PMID: 34556297.
Jing C, Castro-Dopico T, Richoz N, et al. Macrophage metabolic reprogramming presents a therapeutic target in lupus nephritis. PNAS 117 (26):15160-15171, 2020. (Mice). University of Cambridge, National Institute of Arthritis and Musculoskeletal and Skin Disease.
预培养于含有叠氮钠和二抗来源物种正常血清的缓冲液中。 注意:当使用的是带标记的二抗时,千万不能用一抗来源物种的正常血清和 IgG 来封闭。如果血清中的免疫球蛋白非特异性的结合到样品上,他们会被带有标记的二抗识别,导致背景过高。 牛血清白蛋白( BSA )和奶粉是最为常用的封闭液,它们可能含有 IgG, 除了牛抗羊 IgG 外,许多二抗如抗牛,抗山羊,抗绵羊与牛 IgG 有较强的反应。因此,使用 BSA 或奶粉封闭或稀释抗体会增加背景或降低抗体效价。推荐用来自二抗的物种的正常血清( 5% v
® 555 Conjugate)#4409 Anti-Mouse IgG(H+L), F(ab')2 Fragment(Alexa Fluor® 647 Conjugate)#4410 抗大鼠: Anti-Rat IgG(H+L),(Alexa Fluor® 488 Conjugate)#4416 Anti-Rat IgG(H+L),(Alexa Fluor® 555 Conjugate)#4417 Anti-Rat IgG(H+L),(Alexa
源的单克隆抗体,二抗则选抗小鼠的二抗(山羊抗小鼠或者兔抗小鼠等均可);如果一抗是从兔血清里制备的兔源多克隆抗体,则相应的二抗需要选择抗兔的二抗。即根据一抗的物种来源选择相应的抗该物种的二抗。***捷能为您提供最全的抗不同种属的原装进口二抗,包括抗小鼠、大鼠、兔、山羊、绵羊、人、豚鼠、猪、马、牛、鸡、鸭等二抗。 【一抗的类别亚型】 二抗需与一抗的类别或亚类相匹配。这通常是针对单克隆抗体而言。多克隆抗体主要是IgG类免疫球蛋白,因此相应的二抗就是抗IgG抗体。其中单克隆抗体的类别及亚类通常